Difference between Diabetes Type 1 and Type 2
Key Difference: Diabetes Type 1 is characterized by deficiency of insulin in the body caused due to the damage of insulin producing beta cells of Pancreas by the antibodies of the immune system of the body. Diabetes Type 2 is characterized by the body cells getting resistant to the action of insulin and insufficient production of insulin by the beta cells of the Pancreas to subdue the resistance.
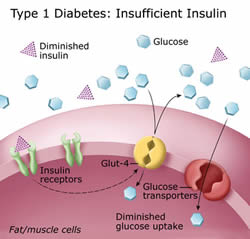
Diabetes is a metabolism disorder that occurs due to improper usage of glucose in the body. The body utilizes glucose with help of insulin which is secreted by the beta cells of the glandular organ Pancreas. Diabetes is caused under two conditions, insulin deficiency (diabetes 1) and insulin resistance (diabetes 2).
 Diabetes 1 is recorded among 5-10% of diabetes patient worldwide while Diabetes 2 is the more common type recorded as 90 -95% the total cases of diabetes.
Diabetes 1 is recorded among 5-10% of diabetes patient worldwide while Diabetes 2 is the more common type recorded as 90 -95% the total cases of diabetes.
Diabetes 1 or Diabetes Mellitus Type 1 is primarily featured by autoimmune basis when the immune system of the body malfunctions and damages the pancreatic beta cells of the islets of Langerhans, diminishing the production of insulin. Insulin controls the glucose usage in the body. The sequential inadequacy of insulin leads to increased level of glucose in blood and urine. Diabetes 1 is commonly found among the adolescence and teen group.
Common symptoms evident in diabetes 1 involve weight loss, excessive hunger or increased thirst, polyuria (frequent urination), abnormal reduction of saliva (xerostomia), bleary vision, fatigue, nausea or vomiting tendencies. The common factors considered to trigger diabetes 1 are environmental factors, polygenic disease (genetic behavior), virus infected cells or dietary reasons.
Diabetes 1 is generally categorized under two sub categories, type 1a which is Latent Autoimmune Diabetes of Adults (LADA) and type 1b. In Type 1a the immune system of the body becomes hyperactive and misidentifies the beta cells as non-self or foreign cells. The controlling T-cells, particularly CD4 and CD8 T cells of the immune system take on an antipathetic role and lead to a pathogenic reflex by intruding the pancreatic islets and destroy the beta cells. Prolonged destruction of the endogenous insulin producing cells leads to a deficiency of insulin in the body. In this type the diabetes can be detected through a laboratory test. If the blood is detected to have markers like islet cell antibodies (ICA), glutamic acid decarboxylase (GAD), antibodies targeting on membranous tyrosine phosphatase. Type 1a is treated with medication; however sometimes require insulin replacement therapy too. Type 1b is recognized when the body cycle requirement for insulin changes.
Diabetes 1 is treated with regular medical management and monitoring of blood sugar and ketone in the blood stream along with a properly monitored diet. The most common and followed treatment is insulin injection or usage of insulin pump to introduce insulin in the body artificially, since insulin is an essential element to maintain a balance of metabolism.
 Diabetes 2 is the more common form of diabetes that has been recorded among diabetes patients. Diabetes 1 is a metabolic disorder mediated due to corresponding insulin deficit and insulin resistance disposition. The body undergoes a dearth of required insulin count to overcome the resistance.
Diabetes 2 is the more common form of diabetes that has been recorded among diabetes patients. Diabetes 1 is a metabolic disorder mediated due to corresponding insulin deficit and insulin resistance disposition. The body undergoes a dearth of required insulin count to overcome the resistance.
The relative symptoms indication Diabetes 2 includes obesity in most cases effectively for those patients affected by genetic disposition. The other prototypal symptoms include frequent urination, increased thirst and excessive hunger. Fatigue, blurred vision, peripheral nervous system disorders are other symptoms recorded often. Certain medications can also predispose to diabetes 2. Apart from genetic factors which records to 80-90% patients having a family member predisposed to diabetes, Diabetes 2 can be attributed to inadequate physical exercise/activity, insufficient diet, mental strain and other lifestyle factors.
Treatment of Diabetes 2 includes regular monitoring of blood sugar and ketone level. The common medical attention for Diabetes 2 includes oral pills, metformin or insulin, dietary control and non-insulin treatments. Controlled diet, minimized intake of sugary drinks and higher dietary involvement of vegetables in diet can be one of the essential prevention measures. However, regular exercise and monitored weight loss or gain can contribute greatly to prevent diabetes risks.
Prolonged high blood sugar level leads to further pathogenic disorders and complexities enhancing common health risk factors like nervous system disorders, cardiovascular diseases, renal failure (kidney failure – which requires dialysis treatment), and visionary disorder due retina damage.
In diabetes 2 insulin resistance co-relates to other medical conditions that often required parallel medical attention like high blood pressure, excess lipid amount in blood and atherosclerosis. Proper medical care in diabetes 2 includes added attention to cholesterol and triglycerides level, hypertension along with glucose level monitoring.
A detailed comparison of basic factors between Diabetes 1 and Diabetes 2:
|
CLASSIFICATION |
DIABETES 1 |
DIABETES 2 |
|
Commonly Known As |
Diabetes Mellitus Type 1, T1DM, Insulin Dependent Diabetes, Juvenile Diabetes |
Diabetes Mellitus Type 2, Non-Insulin Dependent Diabetes Mellitus(NIDDM), Adult Onset Diabetes |
|
What Happens |
Insulin production in body is disrupted as the insulin producing beta cells of the glandular organ Pancreas is destroyed by the autoimmune antibodies in the body. |
Body cells become resistant to regular action of hormone insulin. Glucose level in the blood rises due to increased production of insulin by the beta cells in the Pancreas. |
|
Global Diabetes Prevalence |
More common in European ancestry but found in all ethnic groups equally |
Found more commonly among Africans, Pacific Islanders, Latino, Asian and Native American |
|
Cause |
Environmental, Genetics, Virus Triggered Autoimmune Action, Diet, |
Obesity, Lack of Physical Action, Unusual Glucose Production from Liver, Insulin Resistance, Hyperglycemia, Poor Diet |
|
Symptoms |
Increased Hunger(Polyphagia), Frequent Urination(Polyuria), Fatigue, Blurred Vision, Increased Thirst(Polydipsia), Weight Loss |
Prolonged infection in Bladder, Skin Kidney etc, Increased Urination(Polyuria), Bleary Vision, Erectile Disorder |
|
Diagnosis |
Fasting Plasma Glucose Test, Glucose Tolerance Test, Gycated Hemoglobin Test |
Random Plasma Glucose Test, Fasting Plasma Glucose Test, Glycosolated Glucose, OGTTtest, |
|
Affected Age Group |
Mostly Adolescents
|
Mostly Adults |
|
Onset of Syptoms |
Sudden or Gradual
|
Gradual |
|
Physical Aspect |
Mostly Lean |
Overweight or Obese |
|
Treatment |
Insulin Injection or Insulin Pump, Regular Blood Sugar Monitoring, Controlled Diet |
Regular Exercise, Controlled Diet, Medication (pills or insulin injection) |
Image Courtesy: dtc.ucsf.edu









Add new comment