Difference between Ebola and Marburg
Key Difference: Both the Ebola virus and the Marburg virus are types of the hemorrhagic fever virus that cause severe illnesses in humans. Their symptoms are nearly identical to each other thus making diagnoses difficult.
Both the Ebola virus and the Marburg virus are types of the hemorrhagic fever virus that cause severe illnesses in humans. While the viruses differ from each other, the symptoms of the viral hemorrhagic fever (VHF) as caused by them are quite similar, so much so that their clinical symptoms are indistinguishable from each other.
Both Ebola and Marburg are mainly prevalent in Equatorial Africa; however the diseases can be easily transmitted across borders. In fact, the first noticed case of Marburg was in the German cities Marburg and Frankfurt and the Yugoslav capital Belgrade in the 1960s. Ebola, on the other hand, was discovered in 1976 near the Ebola River in what is now the Democratic Republic of the Congo.
The diseases are often hard to diagnose and are often confused as each other as well as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases such as typhus, cholera, gram-negative septicemia, borreliosis such as relapsing fever or EHEC enteritis, and many others.
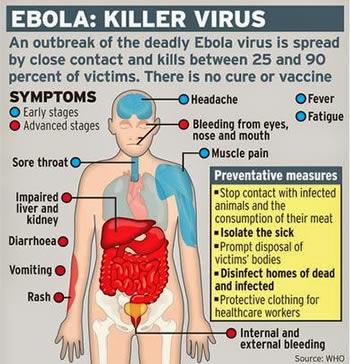
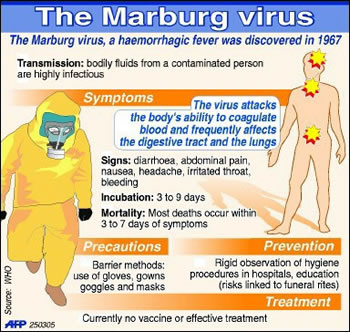 The incubation period of both illnesses is between 2 and 21 days, and the initial set of symptoms is practically identical. The early signs and symptoms include fever, severe headache, joint and muscle aches, chills and weakness. As the patient deteriorates, the symptoms may also include nausea, vomiting, diarrhea, bloody stool, red eyes, raised rash, chest pain and cough, stomach pain, severe weight loss, as well as internal and external bleeding.
The incubation period of both illnesses is between 2 and 21 days, and the initial set of symptoms is practically identical. The early signs and symptoms include fever, severe headache, joint and muscle aches, chills and weakness. As the patient deteriorates, the symptoms may also include nausea, vomiting, diarrhea, bloody stool, red eyes, raised rash, chest pain and cough, stomach pain, severe weight loss, as well as internal and external bleeding.
Both the diseases are transmitted through contract with either their carriers, the bats, or through close contact with the blood, secretions, organs or other bodily fluids of infected animals or other humans.
As the symptoms of both the diseases are nearly identical, the only way to diagnose the illnesses is either through the patient’s travel history (to see if he has been in a risk prone area) or through isolating the virus or the antibodies for the virus in the patient’s blood. However there is still no vaccine for the diseases.
Comparison between Ebola and Marburg:
|
|
Ebola |
Marburg |
|
Known as |
Ebola virus disease (EVD), Ebola hemorrhagic fever (EHF) |
Marburg virus disease (MVD), Marburg hemorrhagic fever |
|
Caused by |
A virus of the family Filoviridae, genus Ebolavirus:
|
Either of the two marburgviruses, Marburg virus (MARV) and Ravn virus (RAVV).
Marburg virus (MARV) is a virus of the Filoviridae family of viruses and a member of the species Marburg marburgvirus, genus Marburgvirus.
Ravn virus (RAVV) is a close relative of the Marburg virus (MARV). |
|
First Discovered |
In 1976 near the Ebola River in what is now the Democratic Republic of the Congo |
In the German cities Marburg and Frankfurt and the Yugoslav capital Belgrade in the 1960s |
|
Natural Hosts |
Fruit bats of the Pteropodidae family |
Old World fruit bats, specifically considered to be Egyptian rousettes (Rousettus aegyptiacus) |
|
Transmission |
|
|
|
Incubation period (the time interval from infection with the virus to onset of symptoms) |
2 to 21 days |
2 to 21 days, averaging 5–9 days. |
|
Symptoms |
Fever, fatigue, muscle pain, headache and sore throat. Followed by vomiting, diarrhoea, rash, symptoms of impaired kidney and liver function, and in some cases, both internal and external bleeding. |
High fever, sudden, severe headache, with accompanying chills, fatigue, nausea, vomiting, diarrhea, pharyngitis, maculopapular rash, abdominal pain, conjunctivitis, & malaise. Followed by prostration, dyspnea, edema, conjunctival injection, viral exanthema, and CNS symptoms, including encephalitis, confusion, delirium, apathy, and aggression, as well as bloody stools, ecchymoses, blood leakage from venipuncture sites, mucosal & visceral hemorrhaging, and possibly hematemesis. The last stage is divided into survivors & fatal cases. Survivors will enter a convalescence phase, experiencing myalgia, fibromyalgia, hepatitis, asthenia, ocular symptoms, & psychosis. Fatal cases continue to deteriorate, experiencing continued fever, obtundation, coma, convulsions, diffuse coagulopathy, metabolic disturbances, shock and death. |
|
Diagnosis |
Confirmation is made using the following investigations:
|
Marburg is clinically indistinguishable from Ebola and can be easily confused with many other diseases. Confirmation is made using the following investigations:
|
|
Treatment |
Rehydration with oral or intravenous fluids- and treatment of specific symptoms, improves rate of survival. |
Treatment is primarily supportive in nature and includes minimizing invasive procedures, balancing fluids and electrolytes to counter dehydration, administration of anticoagulants early in infection to prevent or control disseminated intravascular coagulation, administration of procoagulants late in infection to control hemorrhaging, maintaining oxygen levels, pain management, and administration of antibiotics or antimycotics to treat secondary infections |
Image Courtesy: economicpolicyjournal.com, innov8tiv.com









Add new comment